Rotator Cuff Surgery
- Home
- Rotator Cuff Surgery
Rotator Cuff Surgery
Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the head of humerus (upper arm bone). A partial tear, however, may need only a trimming or smoothing procedure called a debridement. A complete tear is repaired by stitching the tendon back to its original site on the humerus.
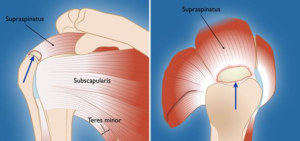
The rotator cuff tendons cover the head of the humerus (upper arm bone), helping you to raise and rotate your arm.
When Rotator Cuff Surgery is Recommended
Your doctor may offer surgery as an option for a torn rotator cuff if your pain does not improve with nonsurgical methods. Continued pain is the main indication for surgery. If you are very active and use your arms for overhead work or sports, your doctor may also suggest surgery.
Other signs that surgery may be a good option for you include:
- Your symptoms have lasted 6 to 12 months
- You have a large tear (more than 3 cm) and the quality of the surrounding tendon tissue is good
- You have significant weakness and loss of function in your shoulder
- Your tear was caused by a recent, acute injury.
The blue arrows indicate a full-thickness tear in the supraspinatus tendon, the most common location for rotator cuff tears.
Surgical Repair Options
There are a few options for repairing rotator cuff tears. Advancements in surgical techniques for rotator cuff repair include less invasive procedures. While each of the methods available has its own advantages and disadvantages, all have the same goal: getting the tendon to heal.
The type of repair performed depends on several factors, including your surgeon’s experience and familiarity with a particular procedure, the size of your tear, your anatomy, and the quality of the tendon tissue and bone.
Many surgical repairs can be done on an outpatient basis and do not require you to stay overnight in the hospital. Your orthopaedic surgeon will discuss with you the best procedure to meet your individual health needs.
You may have other shoulder problems in addition to a rotator cuff tear, such as biceps tendon tears, osteoarthritis, bone spurs, or other soft tissue tears. During the operation, your surgeon may be able to take care of these problems, as well.
The three techniques most commonly used for rotator cuff repair include traditional open repair, arthroscopic repair, and mini-open repair. In the end, patients rate all three repair methods the same for pain relief, strength improvement, and overall satisfaction.
Open Repair
A traditional open surgical incision (several centimeters long) is often required if the tear is large or complex. The surgeon makes the incision over the shoulder and detaches one of the shoulder muscles (deltoid) to better see and gain access to the torn tendon.
During an open repair, the surgeon typically removes bone spurs from the underside of the acromion (this procedure is called an acromioplasty). An open repair may be a good option if the tear is large or complex or if additional reconstruction, such as a tendon transfer, is indicated.
Open repair was the first technique used for torn rotator cuffs. Over the years, new technology and improved surgeon experience has led to less invasive procedures.
All-Arthroscopic Repair
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. The camera displays pictures on a television screen, and your surgeon uses these images to guide miniature surgical instruments.

During athroscopy, your surgeon can see the structures of your shoulder in great detail on a video monitor.
Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions (cuts), rather than the larger incision needed for standard, open surgery.
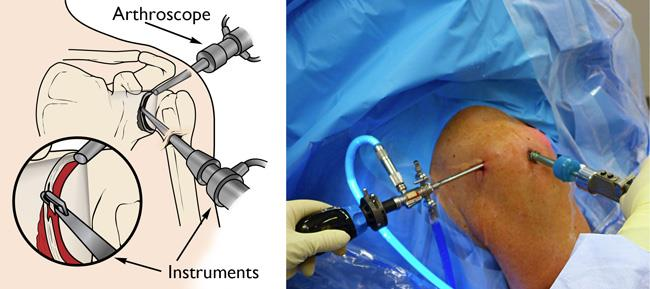
Illustration and photo show an arthroscope and surgical instruments inserted through portals in a shoulder joint.
All-arthroscopic repair is usually an outpatient procedure and is the least invasive method to repair a torn rotator cuff.
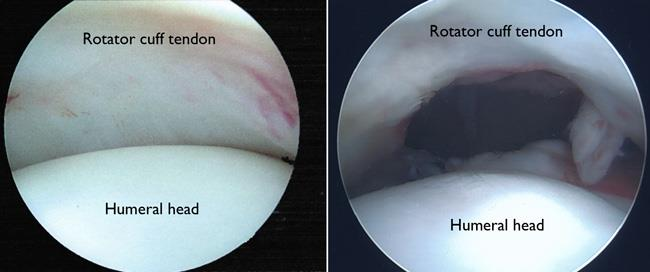
(Left) Arthroscopic view of a healthy shoulder joint.
(Right) In this image of a rotator cuff tear, a large gap can be seen between the edge of the rotator cuff tendon and the humeral head.
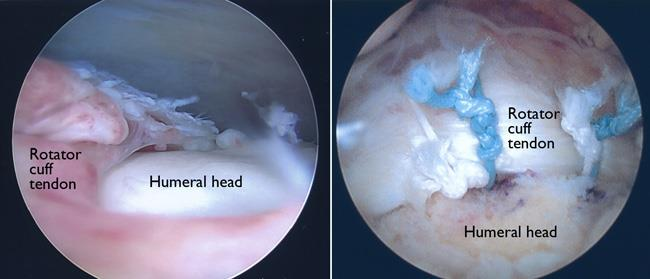
Left) The same rotator cuff tear, as seen from above the tendon.
(Right) The rotator cuff tendon has been re-attached to the greater tuberosity of the humeral head with sutures.
Mini-Open Repair
The mini-open repair uses newer technology and instruments to perform a repair through a small incision. The incision is typically 3 to 5 cm long.
This technique uses arthroscopy to assess and treat damage to other structures within the joint. Bone spurs, for example, are often removed arthroscopically. This avoids the need to detach the deltoid muscle.
Once the arthroscopic portion of the procedure is completed, the surgeon repairs the rotator cuff through the mini-open incision. During the tendon repair, the surgeon views the shoulder structures directly, rather than through the video monitor.
Recovery
Pain Management
After surgery, you will feel pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few weeks after your surgery.
Rehabilitation
Rehabilitation plays a vital role in getting you back to your daily activities. A physical therapy program will help you regain shoulder strength and motion.
Immobilization
After surgery, therapy progresses in stages. At first, the repair needs to be protected while the tendon heals. To keep your arm from moving, you will most likely use a sling and avoid using your arm for the first 4 to 6 weeks. How long you require a sling depends upon the severity of your injury.
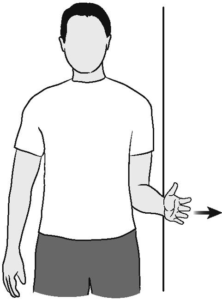
Active exercise during rehabilitation may include isometic external rotation exercises, such as the one shown here.
Passive exercise. Even though your tear has been repaired, the muscles around your arm remain weak. Once your surgeon decides it is safe for you to move your arm and shoulder, a therapist will help you with passive exercises to improve range of motion in your shoulder. With passive exercise, your therapist supports your arm and moves it in different positions. In most cases, passive exercise is begun within the first 4 to 6 weeks after surgery.
Active exercise. After 4 to 6 weeks, you will progress to doing active exercises without the help of your therapist. Moving your muscles on your own will gradually increase your strength and improve your arm control. At 8 to 12 weeks, your therapist will start you on a strengthening exercise program.
Expect a complete recovery to take several months. Most patients have a functional range of motion and adequate strength by 4 to 6 months after surgery. Although it is a slow process, your commitment to rehabilitation is key to a successful outcome.
Outcome
The majority of patients report improved shoulder strength and less pain after surgery for a torn rotator cuff.
Each surgical repair technique (open, mini-open, and arthroscopic) has similar results in terms of pain relief, improvement in strength and function, and patient satisfaction. Surgeon expertise is more important in achieving satisfactory results than the choice of technique.
Factors that can decrease the likelihood of a satisfactory result include:
- Poor tendon/tissue quality
- Large or massive tears
- Poor patient compliance with rehabilitation and restrictions after surgery
- Patient age (older than 65 years)
- Smoking and use of other nicotine products
- Workers’ compensation claims
Complications
After rotator cuff surgery, a small percentage of patients experience complications. In addition to the risks of surgery in general, such as blood loss or problems related to anesthesia, complications of rotator cuff surgery may include:
- Nerve injury: This typically involves the nerve that activates your shoulder muscle (deltoid).
- Infection: Patients are given antibiotics during the procedure to lessen the risk for infection. If an infection develops, an additional surgery or prolonged antibiotic treatment may be needed.
- Deltoid detachment: During an open repair, this shoulder muscle is detached to provide better access to the rotator cuff. It is stitched back into place at the end of the procedure. It is very important to protect this area after surgery and during rehabilitation to allow it to heal.
- Stiffness: Early rehabilitation lessens the likelihood of permanent stiffness or loss of motion. Most of the time, stiffness will improve with more aggressive therapy and exercise.
- Tendon re-tear: There is a chance for re-tear following all types of repairs. The larger the tear, the higher the risk of re-tear. Patients who re-tear their tendons usually do not have greater pain or decreased shoulder function. Repeat surgery is needed only if there is severe pain or loss of function.